Electrophysiology
Electrophysiology is the specialty of cardiology that focuses on the heart’s electrical system. The heart sends electrical signals that controls the rate and rhythm of the heartbeat.
Arrhythmias
An arrhythmia is an irregular heartbeat caused when the electrical signals in the heart don’t function properly. There are several types of arrhythmias including:
Atrial Fibrillation (AFib) With AFib, irregular electrical signals cause the heart’s upper chambers (atria) to beat quickly. The atria quiver instead of fully contracting. As a result blood can pool in the atria instead of moving down into the lower heart chambers (ventricles). This increases the risk of a possible blood clot and stroke.
SVT (Supraventricular Tachycardia) A rapid heartbeat of over 100 bpm, cause by irregular electrical signals, originating in the upper heart chambers (atria). In many cases, people with SVT do not require medical attention. However, prolonged and frequent episodes of SVT may require treatment.
Ventricular Tachycardia (VT) A rapid heartbeat of over 100 bpm, caused by irregular electrical signals, originating in the lower heart chambers (ventricles). This rapid heartbeat can prevent the ventricles from filing up with a sufficient amount of blood to pump out to the rest of the body.
EP (Electrophysiology) Study
During an EP study, an electrophysiologist inserts a catheter (long thin tube) into the patient’s femoral vein in their groin, and guides it to the heart. 3-5 catheters are inserted and placed in different areas inside the heart. These specialized electrode catheters sense the heart’s electrical activity and send signals to EKG monitors. The doctor may send an electrical signal through the catheter to trigger an abnormal heartbeat, so that it can be studied. From the findings of the EP study, the doctor can determine the source and cause of the abnormal heartbeat and decide on the best course of treatment.

Cardiac Ablation
A cardiac ablation is a minimally invasive procedure to treat arrhythmia. An EP study is performed immediately leading up to the Cardiac Ablation. During the cardiac ablation, the electrophysiologist uses a special catheter to apply hot or cold energy to the heart tissue that is producing the abnormal electrical signals. This creates scarring that helps block the abnormal signals and restore a regular heartbeat.
Cardioversion
Cardioversion is used to treat arrhythmia. Patches called electrodes are places on the patient’s chest and/or back, and are hooked to a cardioverter machine. The patient receives medicine through an IV that allows them to go to sleep. During the procedure, the doctor uses the machine to emit low-energy electric shocks to help restore the patient’s heartbeat back to normal.
Pacemaker
A Pacemaker is a small device that helps control abnormal heart rhythms. The doctor places the Pacemaker just under the skin under the collar bone, and connects the device to the heart with electrical leads. The heart of an adult at rest normally beats 60 to 100 times per minute. If the heart starts to beat too slowly (bradycardia), this device produces electrical pulses to restore a normal heart rate. There can be several reasons for the need of a pacemaker but most commonly they are placed to help correct electrical problems that can occur due to age or various other physiological factors.
Defibrillator
An Implantable Cardioverter Defibrillator (ICD) is a device that helps control abnormal heart rhythms. The doctor places the Defibrillator just under the skin under the collar bone, and connects the device to the heart with electrical leads. The heart of an adult at rest normally beats 60 to 100 times per minute. If the heart is beating too quickly (tachycardia), the Defibrillator emits quick, low-energy electrical pulses, called cardioversion, to restore a normal heart rate. If a fatally rapid heartbeat is detected (fibrillation), the Defibrillator emits a powerful electric shock (called defibrillation) to restore a normal heart rate. This device is commonly used for correction of life-threatening ventricular arrhythmias, irregular heartbeats in the lower chambers of the heart that inhibit blood from being pumped properly. Many defibrillators can also now function as pacemakers, emitting low electrical pulses to correct bradycardia, when the heart beats too slowly.
Left Atrial Appendage (LAA)
Atrial fibrillation (Afib) is a type of rapid irregular heartbeat. It can cause blood to pool in an area of the heart called the left atrial appendage (LAA) The LAA is a pouch located off your upper left heart chamber (left atrium). When the blood pools, it can cause clots to form. If the clot escapes from the LAA, it can cut off the blood supply to the brain, resulting in a stroke. Up to 90% of stroke causing blood clots originate from the LAA. Closing off the LAA prevents the clot from escaping, therefore reducing the risk of stroke in patients with Afib not caused by a heart valve problem.
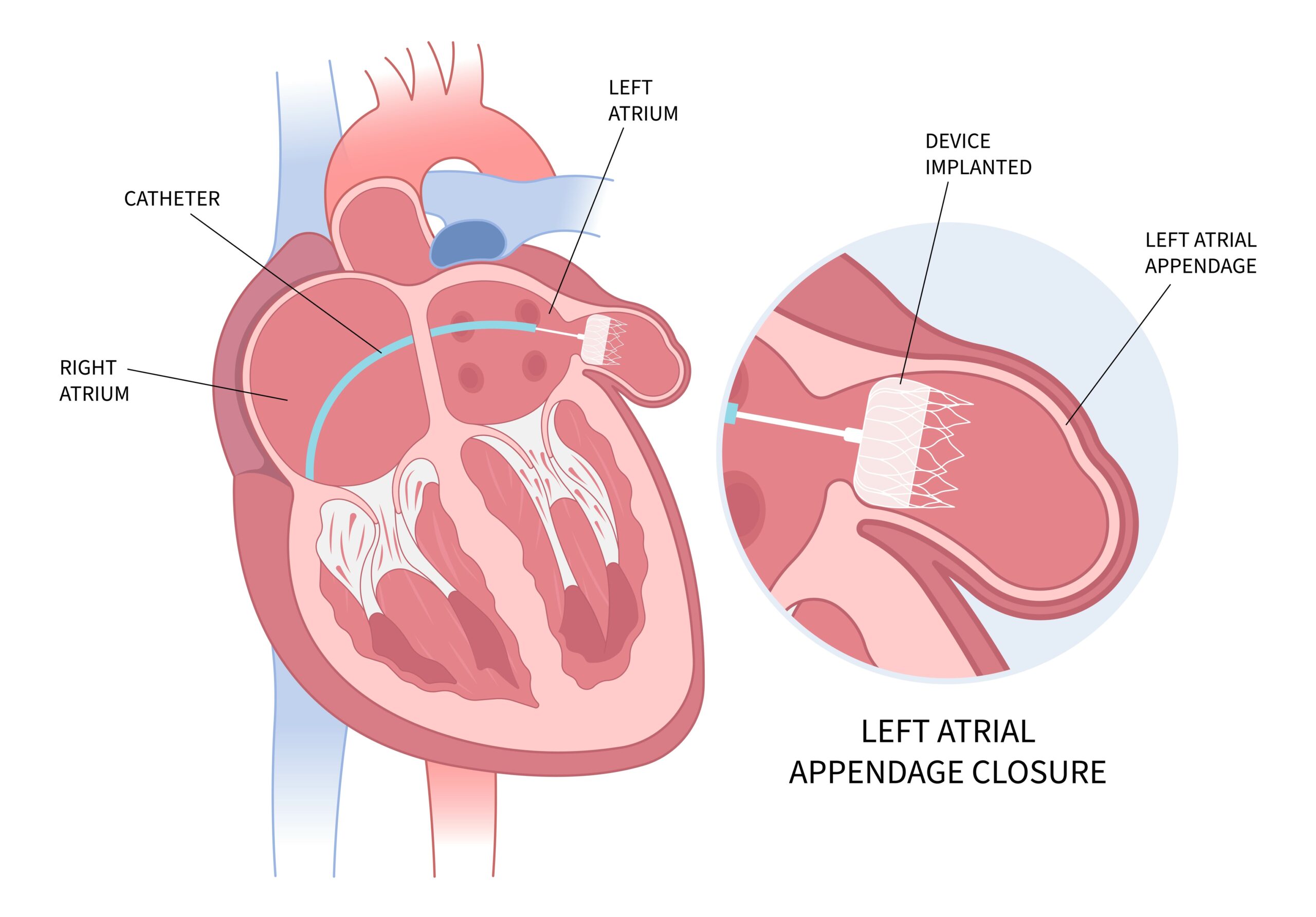
WATCHMAN Device
WATCHMAN is a permanent implant that reduces the risk of stroke for people with atrial fibrillation not caused by a heart valve problem. The WATCHMAN device is the size of a quarter and fits right into the left atrial appendage. It permanently closes off the LAA so no clots will escape.
During this minimally invasive procedure, the doctor makes a small incision in the groin (femoral vein) and advances a long thin tube, called a catheter, up into the heart. The doctor guides the WATCHMAN through the catheter to the LAA. The WATCHMAN is then deployed into the LAA and expands. Once the WATCHMAN is securely in place, the catheter is removed. Over time, a thin wall of tissue grows over the WATCHMAN device to permanently seal off the LAA. Most people are able to stop taking warfarin/blood thinners after 45 days after the implantation. This procedure is done in one of our hospitals by our structural cardiologist.
This procedure offers an alternative to the lifelong use of warfarin without the risk of bleeding that all oral anticoagulants have. WATCHMAN eliminates the need for regular blood tests and food and drink restrictions that come with warfarin/Coumadin.